We hear the far too many tragic stories of children and adults who lose their battle with brain cancer. We hear the remarkable stories of survival where many are able to continue their lives – while not exactly as they lived prior to diagnosis, but can live within society independently, capable, able to work, have families, grow old.
Our story had neither of those outcomes. My husband Matthew was diagnosed with a brain tumour on June Long Weekend 2014. He simply came home from work one day with blurred vision and had experienced a few weeks of tiredness. In the 2 weeks between diagnosis and surgery, Matthew deteriorated rapidly in his sight, speech, cognition and behaviour. On Thursday 26th June, 11 years ago this year, I lost the man I married and had children with to brain cancer. This was the date of his surgery and the man that was wheeled into that surgery, did not come out in any capacity the same man.
Matthew’s tumour was wrapped around his optic nerve and brain stem so the surgery took the best part of a day. He took 3 days to regain consciousness after his surgery and was placed in the Intensive Care unit at JHH. Speaking to Dr Christie in recovery he said that it was a difficult surgery, he thought he was able to remove all of the tumour and that Matt had several strokes during surgery. There was no indication of what was ahead.
There are a few days that are burned into my memory of extremely traumatic events I had to live through during this first year after Matts diagnosis. The first was 6 days after Matts surgery which was also his 45th birthday. Two labcoats walked in and pulled the not-so-cone-of-silence curtain around Matts bed. I was told quite bluntly that Matt had Primary Central Nervous System Lymphoma and he required chemotherapy. They spoke more words but they did not register. Matt burst into tears and started clawing at me. Now Matt was a man that I had never seen any emotion from in the 14 years we had been together – not when our kids were born, not when we got married – NEVER. He was sobbing and making the most awful sounds. Matt had not been able to speak to us post surgery and was looking at me with eyes of a terrified child. This all occurred in front of my 11 year old son Lachlan and 8 year old daughter Emily who had come to see their dad for his birthday. I was overwhelmed with all that was occurring within a space of a few minutes and without any warning – I could feel the walls closing in on me. Protective mode kicked in and seeing the trauma on my kids faces I got them out of there. I drove home after dropping my kids to their friends house. I needed a little time to process and get myself together.
The 2nd traumatic event occurred a few short weeks after when Matt had been transferred from JHH to The Mater. While visiting Matt one day with Emily I was again surrounded by 8 labcoats and given the grim news. I was so distracted during the introductions of all the specialists and staff and what they were telling me as all I could see was my little girl sitting on a chair looking up at us all wondering what was happening to her dad. All I really remember hearing was that Matt required chemotherapy and radiotherapy, Matt was unlikely to survive a few months and if he did, he would be in hospital for at least 6 months. Again, my reaction was to get my kid and get out of there. There was too much to process and this was a far too public place to deal with this information.
Matt was the first patient at The Mater Hospital to be sedated and intubated to receive chemotherapy. It was administered to him over 3 days each cycle and he would be in ICU during this time. Over the weeks post-surgery it had become evident that Matt had suffered severe and life-long brain injuries sustained from his tumour, the surgery and strokes and so much of his independence had been lost. He had no short term memory, was unable to communicate or understand what was occurring with him among many other things. Each time an IV was placed in his arm he would rip it out. When we got to number 26, a team was formed to devise a solution to Matt receiving chemo in a safe manner for him and their staff – hence the regular trips to ICU for this to occur.
After Matts 3rd round of chemotherapy which by now was September, Matt went down hill very quickly with an infection. I left the hospital one night with him happily eating dinner and a few hours later I was called back in as he was rushed to ICU. Over the next 24 hours I watched Matt fight for life as his infection had turned to sepsis which had caused multiple organ failure. I was told late in the afternoon that Matthew was unlikely to survive the next few hours. He was being so heavily supported with countless machines and drugs and standing by his side to watch him fight was traumatic and is an image I will never forget. While the doctors encouraged me to have family bring our kids to the hospital to say goodbye to their dad, I refused. I called them to prepare them for what may happen while in the care of my parents, but they were not entering that ICU to see their dad completely conscious, with those terrified eyes again shake uncontrollably for a few extremely long hours fighting to survive. That was not the last image I wanted them to have of their dad.
Every specialist that worked on Matt that night told me he should not have survived. Each individual issue he was facing was grim, combined, catastrophic. But he did.
Now he did spend those 6 months in hospital between the JHH for a few weeks around his surgery, The Mater for 4 months for his chemotherapy and then several Brain Injury Units for rehabilitation. Over many months Matt learnt to walk again, talk again, feed himself, toilet, shower, dress. Basic needs. While there was so much progress, there were things that would never improve. Matt will always need 24hour supervision and care to cater to his needs.
A few days before Christmas, after 6 months in hospital, we brought Matt home for a few days. Over the next few months we could have him home for weekends and then he would go back to the Hunter Brain Injury Unit at Bar Beach during the week for rehab. Taking him back after that first weekend of having him home was heartbreaking for us all after only having 2 nights home together as a family in 6 months. That broke us again and again each Sunday night we had to return him to care.
Once home full time there were many adjustments our family had to make. We were now living with a completely different man in our home that didn’t look like, sound like or act like he did pre-diagnosis. He was short-tempered, highly emotional, impulsive, child-like in a man’s body. My children and I became full time carers and the busy, sporting, active family we once were, was gone. My children, at 11 and 8, became their dad’s parent – a strange, but very real reality. We were grieving the loss of a man that was physically still here – which was an extremely confusing and difficult process. A process that so many friends and family did not understand as they were all just so happy that he was well and home, which of course we were also – both nothing was the same. Nothing was easy. Every day was a physical, mental and emotional battle and while I had so much support around me, effectively I was alone to manage it all. I no longer had a husband, I no longer had a marriage. It was now just me managing our family. Not having that person that you would share decision making with, share housework with, share parenting with. I tried to parent with what I knew would be Matts perspective and not just my own to try to give them bits of their dad. I had to be good cop and bad cop. I had to be mum and dad. I was managing my own grief, that of my children, and Matts grief from the life that he had lost also. Life was bloody tough. Life was overwhelming.
Throughout all of this I still worked full time as a teacher, cared for our children, managed our home and rental property and our finances. I couldn’t take much time off work as I was now the sole income earner and we still had a mortgage and bills to pay.
The early days of Matt being home were so bloody difficult as he was deeply confused and depressed, rarely wanted to do anything except lay in bed all day and we were all finding it hard to relate as a family again with so much change. There were constant battles each day to get Matt to eat, to take his meds or to shower. He would refuse and either sob or become violent. There were so many times I would be trying to get his meds into him like you would an animal – hide them in his food, trick him to get them in his throat… I had enough to manage than for him to start having seizures on me which would occur if he didn’t have his meds. Countless times he pleaded with me just to let him die. Sometimes now I look back and wonder how I got up each day. I barely slept and our lives were so isolating and difficult, but I did. I did for my kids. They’d lost their dad, I had to keep going for them.
We eventually settled into a routine, Matt improved emotionally with a higher dose of anti-depressants and we secured an NDIS package which provided carers coming into the home to give the kids and I a break. It was such a relief to have some of the physical toll of caring for Matt taken off me as lifting your 80kg husband in and out of a bath each day was no easy feat! Ongoing rehab improved Matts strength and self-help skills further but still today, Matt requires prompting and support to complete every day tasks. He does not feel hunger so he won’t seek food or drink, we have to stand outside the bathroom to verbalise steps involved in showering. He has no short term memory so he could ask us what the date is and 5 minutes later ask us what the date is again. He has poor vision and no downward gaze so when walking with him we always have to prompt him to look down to see in front of him. We listen to the same stories over and over again every day and pretend we are hearing them for the first time. Have you seen the Adam Sandler movie 50 First Dates? Well that’s kind of us.
We’ve had several floods in our house when Matt has turned a tap on to fill the bath and forgotten to turn it off. We had many middle of the night dashes around the neighbourhood to find Matt when he has spontaneously decided it’s a good time to go for a walk. I’ve caught him inches away from dipping his electric shaver in water to clean it as he had it confused with a razor. I had to hide car keys so he wouldn’t hop in the car to drive when he believes he still can. I had to rid the shed of all of his tools after I heard the bandsaw going one day when I dared to leave him for a few minutes to take a shower. Many reasons why he needs 24 hour supervision.
We managed Matt at home for 3 years before it was becoming incredibly evident we were all not in a great place. Matt was becoming so angry and violent, the kids emotional wrecks and well I hadn’t slept in 3 years caring for Matt and my kids while working full time. Things had to change but I just could not bare the thought of placing Matt into full time care. The decision ultimately was made when Lachlan was thrown across the room by his dad one morning and my boy who was trying to be brave, was ultimately terrified so Matt left our home that day and never returned full time. I had to protect the welfare of all 4 members of our family and I knew this was the only way that I could. While it was an easy decision to make in the end, it did not come without complete heartbreak, devastation and the feeling that I was not a decent human being. It took years of therapy for me to be able to live with myself knowing I was the reason Matt no longer lived with us, but I also knew that choice ultimately has us all in a healthier place now. We lost friends and family from that decision and sadly they have not had a relationship with Lachlan, Emily or myself since.
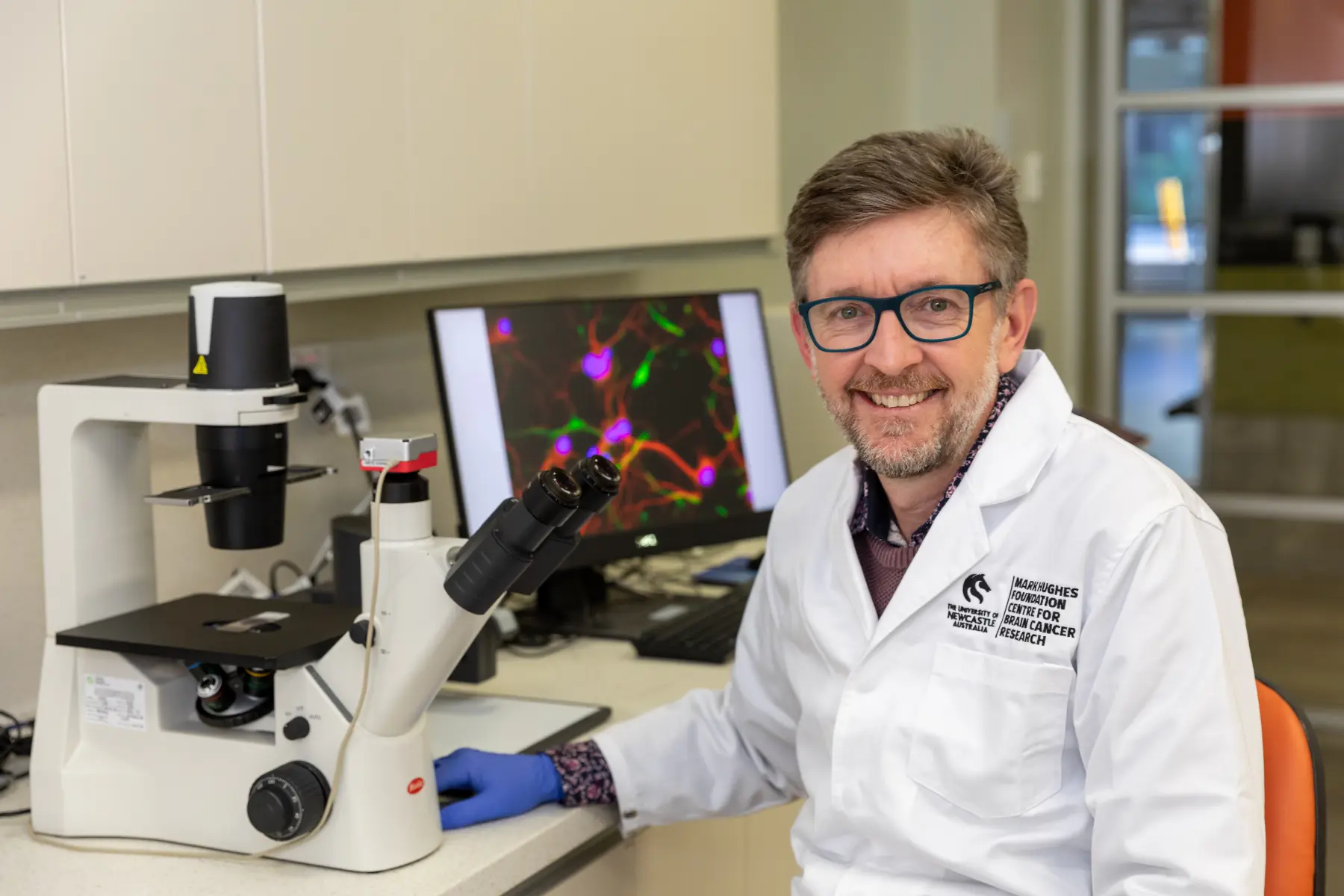
Almost 11 years on from Matts diagnosis, Lachlan is now 22, a cabinet maker and is usually a homebody like his mum. He found it difficult to return to his beloved sport of hockey for the past 10 years, but I can happily say that he has returned to playing this year which I hope he enjoys. Emily is 19, studying Criminology and Law at Newcastle Uni and works as a barrista and barman at The Whistler. She took the loss of her dad the hardest and has had many challenges and hardships over the years which required many years of psychological support. She volunteers with the Mark Hughes Foundation and for many years there you would catch her wearing her beanies all year around! It was a connection to her dad.
Me? Well I have taken a long time to get back into the world, back to playing hockey, feeling like I belong amongst coupled-up friendship groups and getting on with life on my own. I can still find myself at times being emotionally overwhelmed when something triggers me and reminds me of the trauma my family have been through, but these lessen as the years go by. For the 7 years Matt has been in care, we have always had him home every few weekends and we now have him every Monday night for dinner and longer stays over birthdays, Easter and Christmas.
Matt does not hide the fact that he hates me. I have hundreds of love letters (as I call them) detailing his hatred of me cause I’m the wife who threw him out of his house, took his kids away from him and his house and money. That’s how he understands it. I guess that’s the perspective his brain allows. For many years the love letters got to me, now, after many years of my own therapy, I just accept them as Matts way of dealing with his losses of his former life. It’s his therapy.
I had never spoken publicly about the impacts on our family from brain cancer until recently, however, after doing so at MHF events on several occasions now and receiving the overwhelming responses that I have, I understand that it is real-life experiences like these that remind us that we are all ordinary families, the atrocities of brain cancer can hit any one of us at any time and if it does, we are lucky to have the amazing support of the Mark Hughes Foundation to battle it with us. I know that sharing the impacts of brain cancer on our family creates awareness of it devastation and destruction, and hopefully greater support for the foundation.
While it is not unusual to shed tears at MHF events that I volunteer for like the Magic Ball or selling beanies at stadiums over Beanie round when talking to others who have endured the impacts of brain cancer, it is also a little therapy for us all knowing that we are not alone, even though for most of it you feel like you are. While it is a community you never want to be part of, it also feels like the only place you really belong because they emphatically understand what you have and continue to endure.
We are so thankful for Mark, Kirralee and the MHF team for the work they do in our community, so to have the opportunity to join 18 other women on the Southern Alps challenge to raise awareness and money was something Emily and I could not pass up. It will be an amazing experience for my daughter and I to do together – our first trip overseas! While we know our bodies will be tested and we will be sore, and it will be emotional sharing our experiences, it will also be an adventure we will cherish and maybe heal just a few of our wounds. We set ourselves a target of $15,000 to raise prior to leaving for New Zealand and although we’ve reached that target, would love it to continue to grow. We don’t want other families to endure what we have. We don’t want more children to grow up without their parents. We don’t want more parents losing their children. Brain cancer is so cruel, so devastating, so debilitating. If sharing our experience leads to greater awareness and money raised then I will continue to share it and support Mark, Kirralee and the girls at MHF in any way that I can. It’s far too important not to.
You can support Janine and Emily’s fundraising here.