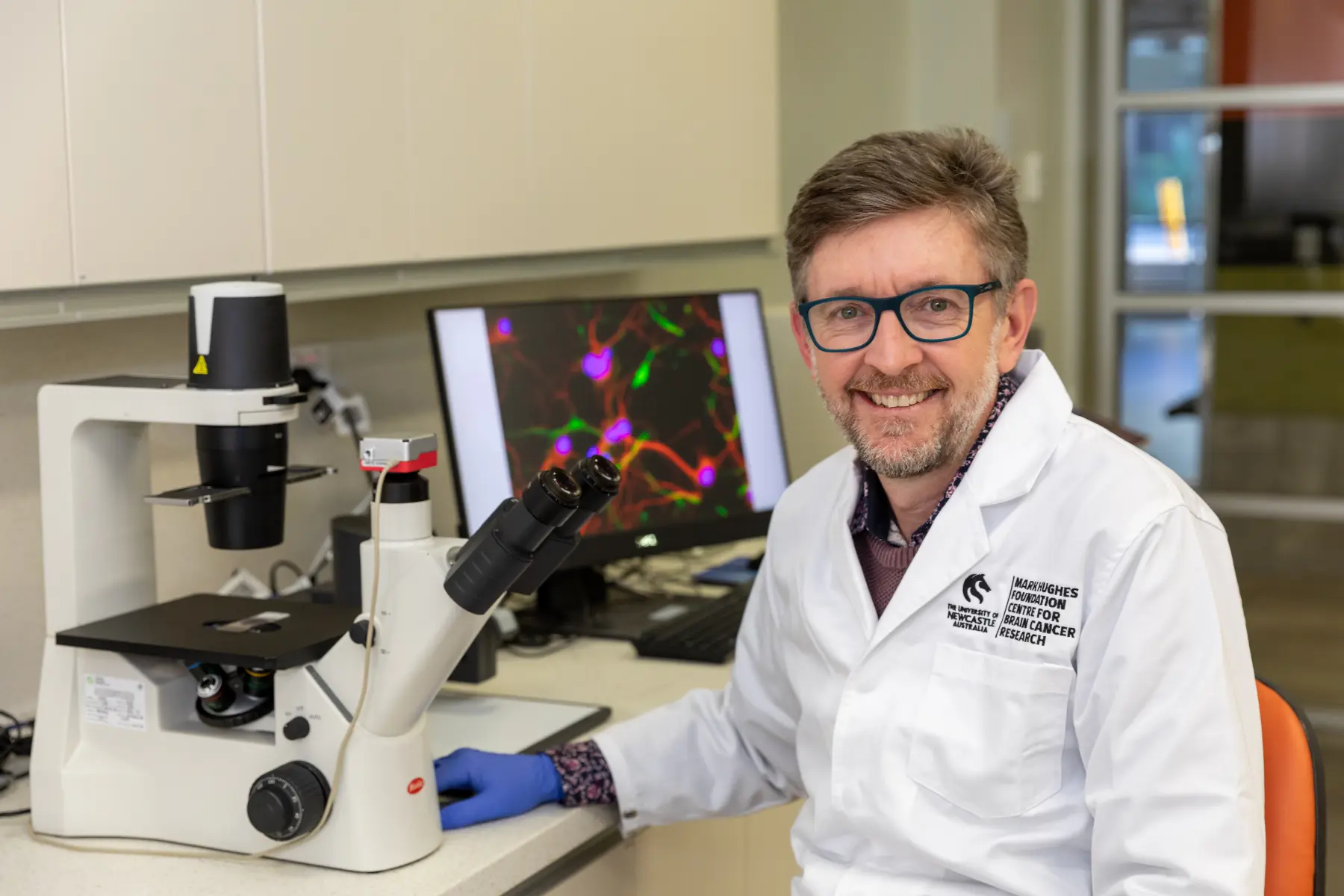
We would like to congratulate Martin Hong, Lucy Leigh, Connor Ballinger, Penny Reeves, Alisha Gooley, Sandy Nixon, Chris Paul and James Lynam on having published this research article showing the impact that the amazing Mark Hughes Foundation funded Brain Cancer Care Coordinators have not only for patients, their loved ones and clinicians but also the health system overall.
These philanthropically funded nurses provide great benefit to our health services and further funding is vital to provide this service to all those living with and effected by Brain Cancer.
Full Paper Published on Oxford Academic
Background
Cancer care coordinators (CCCs) are recognized as having an important role in patients’ and carers’ cancer journey. However, there are no studies investigating the impact of CCCs on quantitative outcomes. We performed a retrospective cohort study investigating the impact of brain cancer care coordinators (BCCCs) on health service resource use and survival in patients with glioblastoma.
Methods
All patients diagnosed with glioblastoma between 2012 and 2019 in Hunter New England Local Health District, Australia (HNELHD) were included and the patients were divided into 2 cohorts: before and after the introduction of the BCCC. Any patient diagnosed in 2016, during the introduction of the BCCC, were excluded. The main outcomes assessed were overall survival, health service resource use, odds of being admitted to hospital after the emergency presentation, and cost-offset analysis to examine the economic implications of BCCCs.
Results
A total of 187 patients were included. There were no significant differences in overall survival between the 2 groups (mOS 12.0 vs 11.16 months, HR 0.95). However, there was a reduction in the number of ED presentations and admissions. This was associated with a 24% reduction in aggregate length of stay with the BCCC. There was no statistically significant difference in mean patient costs, however our hospital may have saved over AUD$500 000 with BCCCs.
Conclusions
The introduction of BCCC did not improve survival but appeared to be associated with reduced health resource utilization. This study provides economic justification, in addition to the established quality of life improvements, to support the presence of BCCCs.